Gum Recession: Why a Few Millimeters Can Change Your Whole-Body Health
Dr. Karen Plymel, Functional Medicine Expert
Most people assume gum recession is simply cosmetic—an aging smile, a little root showing. But this assumption misses the real danger. Gum recession is one of the clearest markers of oral-systemic disease, and it silently fuels inflammation throughout the body.
Mainstream dental associations provide little to no public education on the systemic risks of periodontal disease. As physicians, we must challenge our patients’ understanding: gum health is not just about teeth, it is a biomarker for cardiovascular, metabolic, neurologic, and oncologic health.
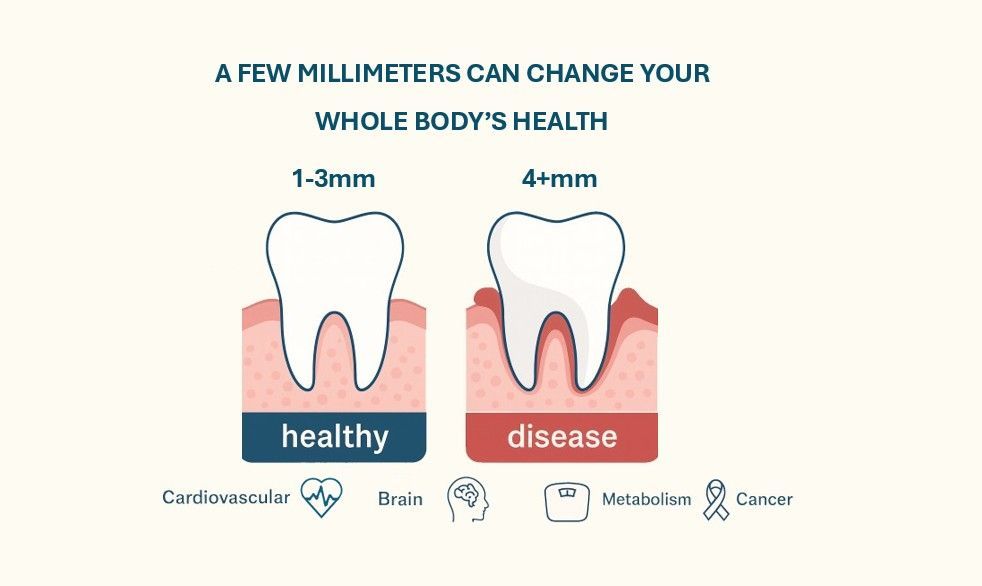
What Gum Measurements Actually Mean
Dentists and periodontists measure the space between gum and tooth using a probe, recorded in millimeters (mm).
- 1–3 mm: Considered physiologic health. The gingiva remains tight to the tooth, protecting underlying bone and roots.
- 4+ mm: This depth is pathologic. It allows anaerobic bacteria, biofilms, and pathogens to invade a niche inaccessible to brushing and flossing, resulting in a self-sustaining infection that enters systemic circulation .
Every millimeter matters. A “4 mm pocket” is not just one more millimeter—it is the difference between health and chronic infection.
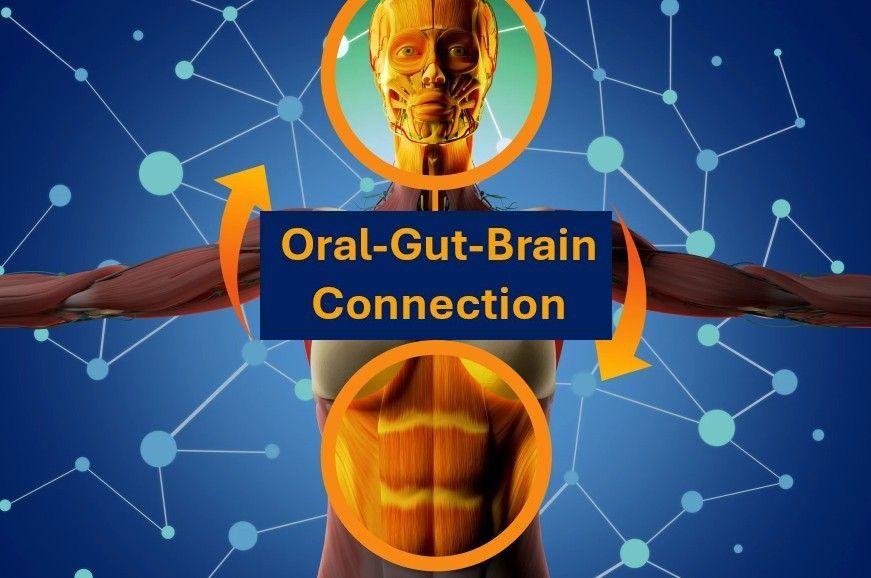
The Oral-Systemic Connection
Periodontal inflammation and oral pathogens act as reservoirs for systemic disease. Once these bacteria and their inflammatory byproducts translocate into circulation, they contribute to multisystem pathology.
1. Cardiovascular Health
Periodontitis is an independent risk factor for myocardial infarction, stroke, and atherosclerosis . Oral pathogens (Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans) accelerate arterial plaque formation and promote endothelial dysfunction.
2. Brain Health
P. gingivalis DNA and gingipain enzymes have been identified in Alzheimer’s brain tissue . Chronic oral inflammation drives neuroinflammation, microglial activation, and cognitive decline.
3. Metabolism & Weight
Periodontal disease worsens insulin resistance and raises HbA1c levels . Treating gum disease can improve glycemic control in type 2 diabetes. Inflammation originating in periodontal tissues can also contribute to obesity-linked metabolic syndrome.
4. Cancer Risk
Chronic periodontal infection is associated with increased risk of pancreatic cancer, oral cancers, and colorectal cancer . Oral pathogens trigger systemic oxidative stress and immune dysregulation, creating a permissive environment for malignancy.
5. Whole-Body Inflammation
Gum recession is not isolated—it is a visible, measurable marker of systemic inflammatory burden. If it is present in the gingiva, it is likely occurring in the vascular endothelium, liver, pancreas, and brain.
Challenging the Patient Mindset
When a patient hears, “You’ve lost a little gum attachment,” it must not be minimized. As clinicians, we should ask:
- Would we ignore a chronic, non-healing wound on the skin?
- Would we dismiss an infection that persists for years?
- Why should gum disease—an infection we can measure in millimeters—be treated differently?
The truth is simple: gum recession is a chronic wound and a marker of systemic inflammatory disease. Ignoring it allows the body-wide consequences to accumulate.
Clinical Implications
- Periodontal probing must be routine and explained to patients with medical significance, not just dental relevance.
- Oral microbiome interventions—including probiotics, targeted antimicrobials, and biofilm disruptors—should be part of systemic health protocols.
- Systemic screening is mandatory in patients with periodontal disease: advanced lipid panels, inflammatory markers (hs-CRP, Galectin-3, TGF-β1), and glucose/insulin assessments.
- Collaborative care between functional medicine providers and airway-focused dentists is essential for whole-body prevention.
Conclusion
- 1–3 mm = health
- ≥4 mm = chronic infection with systemic consequences
From cardiovascular disease to neurodegeneration, from weight gain to cancer risk, gum recession is not cosmetic—it is a medical biomarker. It is time to stop treating periodontal disease as a “dental problem” and start addressing it as a systemic disease.
References
- Tonetti, M. S., & Jepsen, S. (2013). Clinical and biological importance of periodontal attachment loss. Periodontology 2000, 62(1), 1–4.
- Lockhart, P. B., et al. (2012). Periodontal disease and atherosclerotic vascular disease: Does the evidence support an independent association? Circulation, 125(20), 2520–2544.
- Tonetti, M. S., & Van Dyke, T. E. (2013). Periodontitis and atherosclerotic cardiovascular disease. Consensus report of the Joint EFP/AAP Workshop. Journal of Clinical Periodontology, 40(s14), S24–S29.
- Dominy, S. S., et al. (2019). Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Science Advances, 5(1), eaau3333.
- Preshaw, P. M., et al. (2012). Periodontitis and diabetes: A two-way relationship. Diabetologia, 55(1), 21–31.
- Michaud, D. S., et al. (2016). Periodontal disease, tooth loss, and cancer risk. The Lancet Oncology, 17(5), e254–e263.