Is the Mouth the Missing Piece in Your Health?
Dr. Karen Plymel, Functional Medicine Expert

In functional and integrative medicine, we often focus on gut health, hormone regulation, cardiovascular risk, or neuroinflammation. Yet, one of the most overlooked drivers of systemic illness may be hidden in plain sight: the mouth.
Emerging research—and my own clinical experience—shows that unresolved dental issues, jawbone infections, and oral microbiome imbalances can perpetuate chronic inflammation, immune dysregulation, and systemic symptoms such as fatigue and brain fog. Importantly, these issues often remain undetected by standard dental exams.
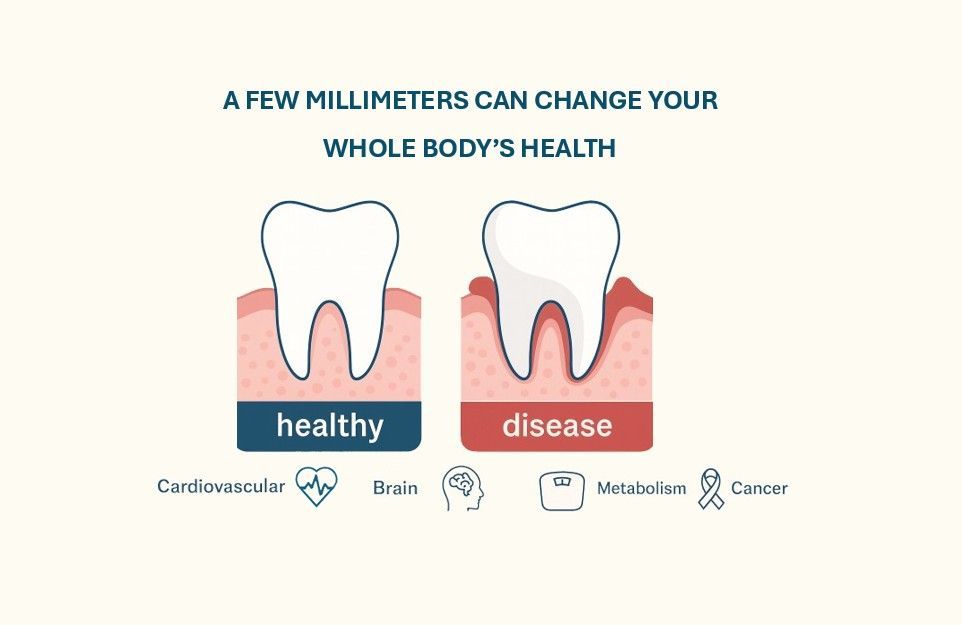
Why Oral Health Impacts the Entire Body
The oral cavity contains more than 700 microbial species, many of which are symbiotic. But dysbiosis in this community can have far-reaching effects:¹ ²
- Digestion & Nutrient Absorption – oral enzymes and microbial activity initiate gut function.
- Nitric Oxide Metabolism – oral bacteria regulate vascular tone and blood pressure.
- Immune System Activation – chronic low-grade infections can prime systemic inflammation.
- Hormone & Neurological Pathways – oral dysbiosis has been linked to brain fog, mood disorders, and hormonal disruption.
When imbalanced, the oral microbiome has been implicated in:
- Cardiovascular disease and vascular inflammation
- Autoimmune disorders
- Chronic fatigue and neuroinflammation
- Hormonal dysregulation
- Sinus congestion and sleep-disordered breathing
The oral-systemic connection is no longer theoretical—it is well documented.¹ ²
Oral Pathogens and Cardiovascular Disease
More than 50% of bacteria linked to cardiovascular disease originate in the mouth. Pathogens such as:
- Porphyromonas gingivalis
- Fusobacterium nucleatum
- Streptococcus sanguinis
have been identified in coronary plaques, where they drive atherosclerosis and vascular inflammation.³ This microbial translocation underscores why oral health is inseparable from cardiovascular, neurological, and immune health.
Why Standard Imaging Often Falls Short
Conventional dental x-rays may overlook deeper pathology, including:
- Root tip infections
- Cavitations (chronically infected or hollow bone defects)
- Osteonecrosis
- Sinus and airway structural abnormalities
These silent pathologies can maintain systemic inflammation even in patients who appear “dentally stable.”
To address this, I rely on Cone Beam CT (CBCT) imaging, which provides a detailed 3D evaluation of teeth, jawbone, and sinuses. I also collaborate with BeamReaders, independent oral and maxillofacial radiologists, for precise interpretation—an essential step in identifying oral-systemic pathology.⁴
Cavitations: The Hidden Reservoir
Cavitations are areas of chronically infected bone, often following extractions or failed root canals. They may remain asymptomatic yet harbor bacteria and fungi that influence systemic disease. Literature links cavitations to:
- Autoimmune illness
- Chronic fatigue and fibromyalgia
- Cardiovascular inflammation
- Neurodegeneration
- Orofacial pain, tinnitus, and sinus dysfunction
Even CBCT can miss cavitations without radiologists trained in subtle interpretation.⁴ ⁵
Root Canals and Systemic Risk
Root canals can preserve natural dentition but create unique challenges. Once devitalized, immune surveillance is compromised. Studies suggest 30–50% of root canals harbor persistent low-grade infection, which can spread to bone or enter systemic circulation.⁶
While not all root canals are problematic, re-evaluation is critical in patients with chronic, unexplained multisystem symptoms.⁷
Closing the Oral-Systemic Gap
Medical and dental education remain siloed:
- Medical training focuses only on oral anatomy, rarely function or pathology.
- Dental training emphasizes teeth and gums, often with minimal systemic integration.
This leaves clinicians with a blind spot in evaluating patients with multisystem chronic illness. At Elevate Health, we bridge this gap through collaboration with airway-conscious dentists, oral-systemic specialists, and integrative practitioners.
Practical Steps for Clinicians
When systemic inflammation or chronic illness remains unresolved, consider oral contributions:
- Order oral microbiome testing (Bristle Oral Biome Test) for patients with systemic symptoms.
- Use CBCT imaging with expert radiology interpretation for hidden infections.
- Avoid overuse of antibacterial mouthwashes that disrupt microbial balance.
- Review patient history of extractions, root canals, or wisdom teeth surgery.
- Integrate whole-mouth health into your chronic disease management protocols.
- Obtain perio-path charting for review
Conclusion
Oral health is more than preventing cavities. It is a critical determinant of inflammation, immunity, cardiovascular function, and brain health. Hidden jawbone infections, cavitations, and oral pathogens may be the missing piece in patients with unresolved chronic illness. By advancing beyond routine dental exams and incorporating CBCT, oral microbiome testing, and cross-disciplinary collaboration, we can improve outcomes for complex patients. At Elevate Health, our mission is to help uncover these overlooked connections—because true whole-body wellness often begins in the mouth.
References
- Willis JR, Gabaldón T. The Human Oral Microbiome in Health and Disease: From Sequences to Ecosystems. Microorganisms. 2020;8(2):308. doi:10.3390/microorganisms8020308
- Kilian M, Chapple ILC, Hannig M, et al. The oral microbiome – An update for oral healthcare professionals. British Dental Journal. 2016;221(10):657–666. doi:10.1038/sj.bdj.2016.865
- Han YW, Wang X. Mobile microbiome: oral bacteria in extra-oral infections and inflammation. J Dent Res. 2013;92(6):485–491. doi:10.1177/0022034513487559
- Bouquot JE, Roberts AM, Person P, Christian J. NICO (Neuralgia-Inducing Cavitational Osteonecrosis): Osteomyelitis in 224 jawbone samples from patients with facial neuralgia. Oral Surg Oral Med Oral Pathol. 1992;73(3):307–319. doi:10.1016/0030-4220(92)90295-Y
- Sharma D, Sreedevi J, Arun AV, et al. The role of cavitational osteonecrosis in oral-systemic disease: A review. J Contemp Dent Pract. 2013;14(2):363–368. doi:10.5005/jp-journals-10024-1337
- Siqueira JF, Rôças IN. Microbiology and treatment of endodontic infections. Endod Topics. 2014;30(1):3–22. doi:10.1111/etp.12029
- Nair PN. Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med. 2004;15(6):348–381. doi:10.1177/154411130401500604